Singapore is poised to achieve at least 80–85 percent vaccine coverage against SARS-CoV-2 by the end of September 2021. Excluding children aged 12 and below, this would mean that at least 90–95 percent of the eligible population are vaccinated. However, is it enough to allow the island state to open its border and resume global economic connection?
When SARS-CoV-2 arrived in Singapore in January 2020, it was among the few countries in Asia to confront the first wave of imported cases. Local transmission ensued. At the epidemic’s peak, Singapore reported approximately 1,000 cases a day, leading to a whole-of-government approach to contain the virus through coordinated policy setting and implementation of strict prevention measures. These included the partial lockdown of the city-state, contact tracing, quarantine, and ramping up of testing and isolation facilities. In this COVID-19 pandemic, Singapore has placed great emphasis and reliance on vaccination. Investment in vaccine research and procurement paid off as Singapore became the first Southeast Asian country to roll out the vaccination in December 2020.
There are several key learning points. First, the state of preparedness stems from past experiences of novel pathogens, which led to hefty investment in constructing the National Centre for Infectious Diseases. This state-of-the-art isolation-treatment facility integrates clinical care with public health testing, epidemiology, research, and community engagement, as well as the ability to mobilize the entire health-care system, including the public-private sector, from primary care to critical care.
Second, the government of Singapore was committed to containing the disease, which achieved the objective of saving both lives and livelihoods. The provision of more than 30,000 beds in community isolation facilities in barely five weeks was the result of a national effort. SGD 93 billion was also set aside in stages for relief measures to buffer the negative impact on the economy. Last but not least, trust in the government and the community’s resilience were instrumental in maintaining social stability and cohesiveness.
The government of Singapore was committed to containing the disease, which achieved the objective of saving both lives and livelihoods.
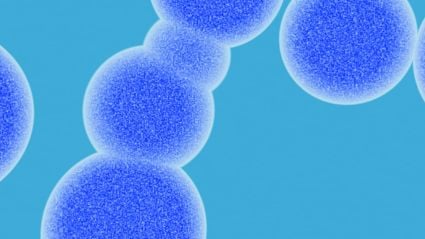
The low number of COVID-19 cases was unfortunately punctuated by the Delta variant in April 2021. Within a week or two, it became the dominant variant. Its biological characteristics were surprisingly different from its origin. We were astonished to find high quantities of viral materials in respiratory secretions through PCR tests, amounting to approximately 1,000-fold greater than with the original strain. We found shorter serial intervals, where the addition of both factors suggested higher transmission capacity in a shorter time frame. We perceived that we were heading into a different phase of the battle against SARS-CoV-2. The clinical characteristics of the Delta variant also changed, where more patients across age groups developed pneumonia, requiring supplementary oxygen. Blood samples from various cohorts of vaccine recipients and community seroprevalence studies showed reduced neutralization of antibodies against the Delta variant and progressive waning of antibodies. Clinical cases of post-vaccination infection started appearing, mostly affecting older age groups. A household contact study showed that vaccine effectiveness is approximately 60 percent in preventing all forms of SARS-CoV-2 infection.
Generally, the vaccine retains its effectiveness in patients with serious illness. However, with the estimated R0 (i.e., the number of new infections estimated to stem from a single case) of 5.8 according to the US Centers for Disease Control and Prevention, herd immunity solely by vaccination has become unattainable. The number of cases is expected to rise. However, it remains to be determined whether herd protection against serious infections is achievable. Equally, the question arises of whether the volatile regional and global COVID-19 situation could impede transition from a pandemic to an endemic stage.
It remains to be seen whether Singapore can find its own path toward an endemic stage without crippling its healthcare system and shattering the confidence of its society. Would Singaporeans welcome a progressive easing of mobility restrictions, moving from hospital-centric to home/community-centric care? Israel, which has similar vaccination strategies, could perhaps be a reliable case study for Singapore. Would a booster dose or annual vaccination, as for influenza, be the way forward?
Moving into an uncharted area, Singapore needs to rely on several key factors: preparing the community in every step of implementation with frequent engagement; giving clear, consistent messages; promoting research and continuing to let science inform policy; being vigilant and adaptable; shifting the responsibility for COVID-19 containment from the government to the individual and community. This last step would require universal masking, self-regulated mobility restrictions, social distancing, environmental and hand hygiene, and awareness of personal health-seeking behaviors. Compared with the seasonal influenza, knowledge of SARS-CoV-2 is currently incomplete. The longer-term harm of SARS-CoV-2 to health is undetermined, and this is no time to be complacent. Regardless of transition stage, it is the responsibility of every Singaporean to avoid SARS-CoV-2 infection.